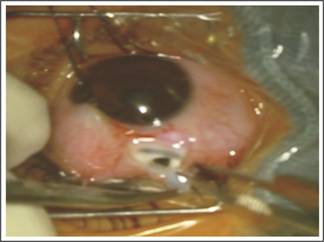
Fig. 1: Pre-
operative Scleral thinning after traumatic scleral perforation with a Nail.
DISCUSSION
The main
outcome in our study was a stable ocular surface in patients who received scleral patch grafting after spontaneous and traumatic
corneoscleral perforations. Previous report shows that corneal and
corneoscleral injuries are well known major cause of decreased vision and
ensuing decrease in quality of life for service members16. In our
study, human homograft and autograft techniques were used as it is used to
manage ocular diseases reported in earlier study17.
In our study, patients were found with trauma at initial
visit and were treated with scleral patch grafts in spontaneous and traumatic
corneoscleral
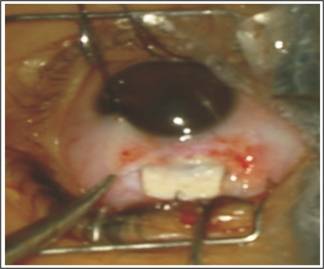
Fig. 2: Postoperative picture showing
scleral thinning strengthened by a scleral patch graft.
perforations similar to
many other studies2,18. The biological quality of corneoscleral
discs was reported comparable to that of tissue obtained from enucleated eye. Sclera
(corneoscleral button) has number of advantages but the strict criticism was
necrotic process. Similarly, peripheral corneal grafting is also the rare
surgical treatments with tectonic sclera excluding
in case of necrotizing sclera19. Sclera was also used as a
graft in most of the studies, in scleromalacia. Similarly, there is a list of many
tissues used as reconstructive materials but, still no such material is universally
acceptable.

Fig. 3: Severe corneal thinning with
descemetocele covered with scleral patch graft.
In our study,
males are more commonly affected than females similar to Shalini Mohan et.al.
study in which five times more affected peoples are males than females15.
The risk of damage was commonly found in young age group – around half of patients
in our study were under 50 years of age. Detailed patient data which includes
mode, duration and injury object are foremost step followed in any corneoscleral
perforation repair. But, it was included in limitations of our study that no
such related history was noted from patients. Patients before surgery were properly
evaluated to the injury with other associated injuries for possibility of
concomitant microbial contamination etc.
It is well
known that surgical treatment alone does not solve the problem of the patient,
therefore physician must control the immunoregulatory dysfunction which causes destruction
of the graft and, subsequently, the patient's eye20.
After scleral
graft visual acuity was improved in our study similar to study done by Hwan and
coworkers21. Previous studies show that visual improvement was made
by removing sutures on corneal side of scleral graft and by decreasing
inflammation22. Ti et al, reported that after pterygium surgery in
patients with scleral melting, corneal lamellar graft help to maintain
integrity of the globe23. In this study, scleral patch grafting in
spontaneous and traumatic corneoscleral perforations was achieved in most of
the eyes for scleral defects of favorable structural outcome. Only, three
patients had complications; two patients developed phithisical eye and one eye
was eviscerated due to late onset endophthalmitis.
This study has numerous limitations, including the loss of
patients to follow-up and incomplete records. Despite the numerous limitations,
the study demonstrates the limitations of our current surgical capabilities to combat
ocular trauma. Another limitation is the lack of details of re-epithelialization
of the stable ocular surface.
CONCLUSION
This
study concludes that preserved scleral graft in
spontaneous and traumatic corneoscleral perforations provides functional and
structural stability to eyes with rare complications.
Conflict of Interest
There is no conflict of
interest.
Author’s Affiliation
Dr. Sharjeel Sultan
MBBS, DOMS, MCPS, FCPS, FRCS.
Assistant Professor Ophthalmology
Dow University of Health Sciences
Civil Hospital, Unit 2 Eye Department Karachi-Pakistan
Dr. Nisar A Siyal
MBBS, MCPS, FCPS
Assistant Professor Ophthalmology
Dow University of Health Sciences
Civil Hospital, Unit 2 Eye Department Karachi-Pakistan
Dr. Nargis Nizam Ashraf
MBBS, FCPS.
Assistant Professor Ophthalmology
Dow University of Health Sciences
Civil Hospital, Unit 2 Eye Department Karachi-Pakistan
Dr. A Rasheed Khokhar
MBBS, FCPS
Professor and Head of department ophthalmology
Dow University of Health Sciences
Civil Hospital, Unit 2 Eye Department Karachi-Pakistan
Role of Authors
Dr. Sharjeel Sultan
Concept and design, undertook the data analyses, wrote, edited and
revised the manuscript.
Dr. Nisar A Siya
Interpretation of data, wrote and
reviewed the manuscript
Dr. Nargis Nizam Ashraf
Wrote, edited and reviewed the manuscript
Dr. A Rasheed Khokhar
Reviewed and approved the manuscript
REFERENCES
1.
Jennifer HS, Marian S. M Needles,
Sutures, and Instruments. Available from www.ophed.com
2.
Fong YY, Yu M, Young AL, Jhanji V. Presentation and management outcomes of corneal
and scleral perforations in geriatric nursing home residents. Medicine, 2015; 94
(36).
3.
Shalini M, Anand A, Anita P, Shibal B. Repair of Corneoscleral Perforations. DOS Times– 2008; 14 (2).
4.
Dandona R, Dandona L.
Corneal blindness in a southern Indian population: need for health promotion strategies.
Br J Ophthalmol. 2003; 87 (2): 133-141.
5.
Sangwan VS, Jain V, Gupta P. Structural and functional outcome of scleral
patch graft. Eye, 2007; 21 (7): 930-5.
6.
Nguyen QD, Foster CS. Scleral patch graft in the management of
necrotizing scleritis. International ophthalmology clinics, 1999; 39 (1): 109-31.
7.
Parekh M, Ferrari S, Di Iorio E, Barbaro V,
Camposampiero D, Karali M, Ponzin D, Salvalaio G. A simplified technique for in situ excision of
cornea and evisceration of retinal tissue from human ocular globe. Journal of
visualized experiments: JoVE. 2012; (64): 3765.
8.
Sangwan VS, Jain V, Gupta P. Structural and functional outcome of scleral
patch graft. Eye, 2007; 21 (7): 930.
9.
Lee JS, Shin MK, Park JH, Park YM, Song M. Autologous advanced tenon grafting combined with
conjunctival flap in scleromalacia after pterygium excision. Journal of
ophthalmology, 2015; 2015.
10.
Ramenaden ER, Raiji VR. Clinical characteristics and visual outcomes in
infectious scleritis: a review. Clinical Ophthalmology (Auckland, NZ). 2013; 7:
2113.
11.
Sahin I, Alhan D, Nışancı M, Ozer
F, Eski M, Işık S.
Auto-/homografting can work well even if both autograft and allograft are
meshed in 4: 1 ratio. Ulusal travma ve acil cerrahi dergisi = Turkish journal
of trauma & emergency surgery: TJTES. 2014; 20 (1): 33-8.
12.
Ti SE, Tan DT. Tectonic corneal
lamellar grafting for severe scleral melting after pterygium surgery.
Ophthalmology, 2003; 110 (6): 1126-36.
13.
Stunf, S., Lumi, X., & Drnovšek-Olup, B. Preserved scleral patch graft for unexpected extreme scleral
thinning found at the scleral buckling procedure: A case report. Indian Journal
of Ophthalmology, 2011; 59 (3): 235–238.
14.
Elisabeth, P., Hilde, B., & Ilse, C. Eye bank issues: II. Preservation techniques:
warm versus cold storage. International
Ophthalmology, 2008; 28 (3),
155–163.
15.
Yonekawa Y, Chodosh J, Eliott D. Surgical techniques in the management of
perforating injuries of the globe. International ophthalmology clinics, 2013; 53
(4): 127-37.
16.
Vlasov A, Ryan DS, Ludlow S, Coggin A, Weichel
ED, Stutzman RD, Bower KS, Colyer MH. Corneal and corneoscleral injury in combat ocular trauma
from Operations Iraqi Freedom and Enduring Freedom. Military medicine, 2017; 182
(1): 114-9.
17.
Hamdi M, Hamdi I. Scleral Repair by Biodegradable Collagen Implant
in Strabismus Surgery. Ophthalmol Res an Int J. 2015; 3 (4): 141-6.
18.
Repair of Corneoscleral
Perforations (PDF Download Available). Available from:
https://www.researchgate.net/./234059015_Repair_of_Corneoscleral_Perforations.
19.
Nguyen QD, Foster CS.
Scleral patch graft in the management of necrotizing scleritis. International
ophthalmology clinics, 1999; 39 (1): 109-31.
20.
Parada-Vasquez RH, Benitez-Castrillon PC, de
Leon-Ortega JE, Leon-Roldan CR. Scleral patch graft in the management of necrotizing
scleritis with inflammation. A case report. Archivos de la Sociedad Espanola de
Oftalmologia. 2016; 91 (7): 353.
21.
Hwan J, Kim JC. Repair of scleromalacia
using preserved scleral graft with amniotic membrane transplantation. Cornea, 2003;
22: 288–293.
22.
Sangwan VS, Jain V, Gupta P. Structural and functional outcome of scleral
patch graft. Eye, 2007; 21 (7): 930.
23.
Pai V, Shetty J, Amin H, Thomas M. Management of Scleral Thinning: An Alternate
Approach. Nitte University Journal of Health Science, 2016; 6 (1): 88.